On Wednesday 24th September 2025, academics, clinicians, local policy leaders, and the public came together for an afternoon of discussion on the “Future of Low Carbon Health and Care”. The workshop, co-hosted by the Centre for Personalised Medicine, the Global Centre on Healthcare and Urbanisation and the National Institute of Health Research Applied Research Collaboration Oxford and Thames Valley, was held at The Hub, Kellogg College, which as the University’s first Passivhaus building was a fitting setting for the discussions of the day.
The afternoon was opened by Professor Sara Shaw who spoke of the urgent need for low-carbon, climate resilient, and equitable health and care systems. She presented key themes for the workshop ahead; the environmental impact of health and care systems, the health and social harms posed by climate change, the need to ensure continuity of care within climate-resilient health systems, the potential co-benefits of considered climate action, and the moral and ethical imperative to act.
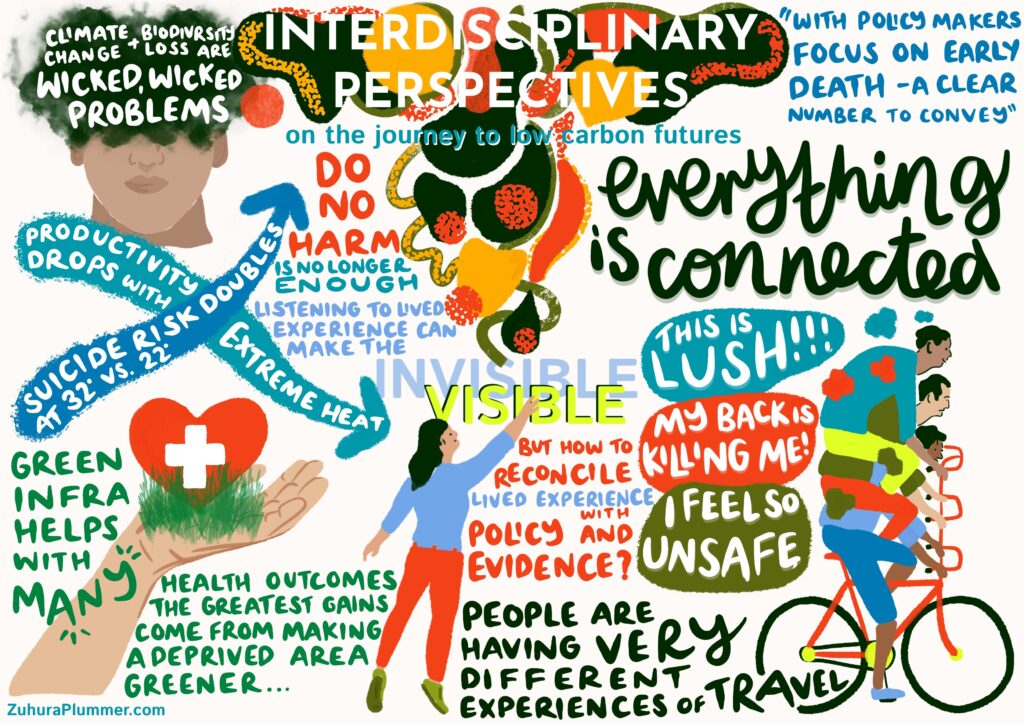
Interdisciplinary Perspectives
The afternoon proceeded with an interdisciplinary panel, chaired by Dr Juliet Carpenter, exploring perspectives on the role and actions of different sectors in limiting environmental impact.
Dr Martha Crockatt introduced her research on the relationship between green infrastructure – the collection of natural spaces that allow people to interact with ecosystems – and population health. Her work demonstrates the co-benefits of green space initiatives: actions that are ecologically beneficial and improve public health outcomes. Yet, she warned of the potential unintended consequences of so-called ‘green gentrification’, characterised by the relocation of higher-income individuals who are attracted by greener neighbourhoods, which can potentially displace local communities.
Continuing this conversation around inclusion and accessibility, Dr Jennie Middleton, presented the work of the ‘Care on the Move’ project, which is examining barriers to everyday mobility and ‘active travel’ by focusing on the physical, emotional, and logistical labour associated with care on the move. She spoke of how assumptions are often made in relation to ‘active travel’, which do not consider lived experience or social inequalities, and provoked discussion around the romanticised ideals of walking in urban imaginaries which exclude many population groups.
Dr Laurence Wainwright brought the role of business to the discussion, calling for a fundamental re-examination of the purpose of business – including how business can work better to ensure environmental responsibility. He drew particular attention to the relationship between extreme heat and mental health to highlight the intersection between environmental stressors, wellbeing and economic resilience, which provided a bridge into the later discussions of the day on the climate-related barriers facing health and care systems.
Health, Care and Climate in Practice
The second panel of the afternoon, chaired by Dr Louisa Chenciner, engaged with the health and care system in relation to the climate crisis.
Speaking of the limitations of focussing solely on the ‘carbon footprint’ in healthcare, Dr Søren Kudsk-Iverson referenced the current policy landscape, with legally-binding NHS commitments to achieve net zero by 2040 for direct carbon emissions. Echoing earlier discussions, he emphasised the need to better address health and social inequalities in the healthcare system alongside efforts toward decarbonisation of core infrastructure.
Subsequently, Dr Sara Khalid shared her work as head of the Planetary Health Informatics Lab. She provided perspectives on the ‘whole-exposome’ approach – which accounts for intersectionality, and how this can be applied to understand the effects of climate change on different population groups. She set out recent work to develop climate risk scores, amid more frequent and severe extreme weather events, and highlighted the need to integrate climate adaptation with mitigation.
Dr Amy Booth provided insights into the supply chains which enable the functioning of health and care systems. She referenced the wide scope of supply chains: from hospital food to medical devices and drugs. Her work encouraged attendees to broaden their perceptions of the environmental impacts of supply chains, beyond carbon footprinting, to consider waste byproducts and the ecological consequences of using natural products in manufacture.
Finally, Dr Pete Sudbury spoke of the need for radical, system-led change, in the face of threatened planetary boundaries. He explored the importance of narratives on climate change, and the potential for collaborative working in this area. Alongside fellow panellists, he advocated for the need to address wider social inequalities and for the NHS to move from sickness to prevention.
The event concluded with reflections from Dr Sarah Briggs, with the display of engaging visual minutes which conveyed key themes of the afternoon’s discussions created by Zuhura Plummer. Sarah spoke of how necessary changes within the health and care system are nested within broader societal and systems change, concluding that environmentally sensitive health and care must go beyond carbon. The evening culminated in a networking reception – a great opportunity to reflect and make new connections.

We are keen to continue work to support ongoing collaboration, research and teaching in this area – if you are working in this or allied areas in Oxfordshire and would like to keep in touch, or if you would like further information about the event, please contact cpm@well.ox.ac.uk.
Louisa Chenciner and Megan Wadsworth